
Expert dental tips, news, and smile advice
Gum Grafting Explained: When It’s Needed, What to Expect, and How to Feel at Ease
Jack’s Story: When a Smile Starts to Shrink

Jack was 42, a runner, and—by his own admission—someone who flossed only when life slowed down. One spring he noticed his front teeth looking longer in his selfies, as if Photoshop had quietly dragged the gumline downward. Soon hot coffee stung along the necks of his lower incisors, and he caught himself covering his smile.
When Jack finally booked an exam, his biggest question wasn’t “Do I need gum grafting?” It was “Am I already too late?” He feared surgery, dreaded a lecture, and assumed recovery would derail his upcoming half-marathon training.
Jack's concerns mirror what we hear every week. Receding gums make people wonder if their mouth is failing—and whether the fix will feel worse than the problem. This post unpacks the why, how, and what-if of grafting so you can decide with clarity and confidence.

Why Gums Recede in the First Place
Recession is often described as “the slow-motion cavity.” You rarely notice its progress until sensitivity or aesthetics nudge you. Common culprits include:
- Aggressive brushing with stiff bristles or horizontal scrubbing
- Periodontal disease that erodes supporting bone
- Thin tissue biotype—some of us are born with delicate gum architecture
- Orthodontic movement that leaves certain roots outside the bone envelope
- Clenching or grinding that flexes teeth at the neck
- Lip or tongue piercings rubbing a constant groove
Left unchecked, recession can expose root surfaces, invite decay, and eventually loosen teeth. That’s why gum grafting is less cosmetic vanity and more structural rescue.
Straight Answer: Gum grafting—technically called soft tissue grafting—is a minor surgical procedure that re-covers exposed roots, usually takes about 45–60 minutes per area, and helps stabilize teeth while reducing sensitivity.

How Gum Grafting Actually Works
Imagine a blanket with one corner folded back. Grafting is like sewing an extra patch beneath that gap, then smoothing the blanket edge over it. Clinically, there are three main approaches:
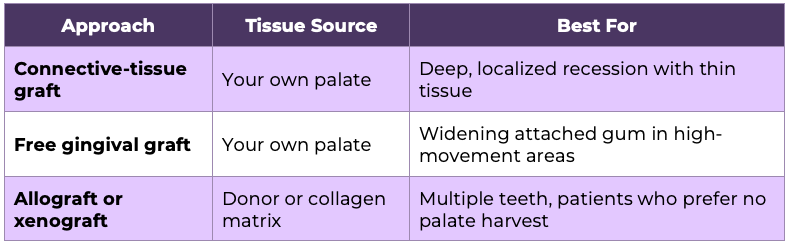
Whichever method your periodontist or trained general dentist chooses, the goal is the same: rebuild a thick, blood-rich collar of tissue around the tooth neck. The added thickness acts like a padded cuff protecting the underlying bone from further erosion.

What to Expect—Step by Step

1. Consultation and Digital Imaging
At your first visit we photograph, probe, and scan your gums. 3-D imaging shows exactly how much bone supports each root. If we see active infection, you’ll complete periodontal therapy first; grafts only succeed in a clean environment.
2. Choosing the Graft Type
We discuss goals—sensitivity relief, aesthetic balance, or both—and weigh whether a palate harvest makes sense. Modern collagen matrices often rival autografts in success, so you have options.
3. Day of Surgery
- Topical anesthetic, then local anesthesia (no general sedation required unless you request it).
- Micro-incisions create a tiny envelope under the recession site.
- The graft slips in like a letter into an envelope; microsutures secure it.
- A light periodontal dressing protects the area.
4. Immediate Recovery
You’ll feel numb for two hours and mildly tender after. Most patients compare it to a scraped knee—not crippling, just annoying. Over-the-counter ibuprofen usually suffices. If we harvested tissue, your palate may feel like a pizza-burn for a week.
5. Long-Term Healing
By day 14 the graft “pinks up,” signifying revascularization. Full maturation takes 6–8 weeks. We’ll see you at one week, six weeks, and six months to photograph progress. Success rates hover around 92–97 percent when done under optimal conditions.
Pro Tip: Sleep with a mouthguard if you grind. Excess pressure is the #1 reason graft margins creep over time.

Emotional Hurdles We Don’t Ignore
Many adults delay grafting because the word “surgery” triggers dread. At Fortson Dentistry in Lathrup Village, we’ve learned that emotional anesthesia matters as much as lidocaine. Here’s what that looks like:
- Transparent visuals: We show before-and-after cases so you can picture your outcome.
- Control cues: You hold a wireless call button; if you need a pause, we stop.
- Guided breathing: Simple box-breathing lowers cortisol, making anesthesia more effective.
- Optional oral sedation: A short-acting tablet taken an hour prior keeps you calm yet responsive.
Jack chose minimal sedation. He later said the scariest moment was the night before—“Once I was in the chair, it felt no different than a filling.”

Cost, Value, and Insurance Realities
Average cost in Michigan ranges $900–$1,600 per tooth depending on graft type and complexity. Most PPO plans reimburse 50–80 percent when recession exposes the root; purely cosmetic grafts rarely qualify.
Think of grafting like foundation repair on a house. Nobody brags about it at dinner, but it prevents costlier disasters—root decay, nerve exposure, or even implants—to the tune of $3,000–$5,000 per tooth later on.
Financing tip: Many patients use HSA or FSA funds because grafting counts as medically necessary once documented. We’ll supply the narrative and photos insurers crave.

Life After Grafting: Habits That Protect Your Investment
- Soft-bristle brushing: Enough pressure to clean a grape without breaking its skin.
- Nightguard if you clench: Custom guards disperse up to 70 percent of bite force.
- 6-month periodontal maintenance: Professional polishing keeps new tissue plaque-free.
- Diet rich in vitamins C and D: Collagen loves these nutrients.
- Mind the retainer: If you’ve had braces, wear it; shifting teeth can torque graft sites.
Jack followed these guidelines. At his one-year review, his graft looked indistinguishable from native gum, and he completed his half-marathon without missing a training day.


FAQ—What Patients Ask Us Most
Q1. Does gum grafting hurt during or after the procedure?
During the surgery you’ll be numb; many patients nap to music. Post-op discomfort is mild to moderate and peaks at 24 hours. At our practice, we send most patients home with ibuprofen 600 mg and an anesthetic rinse. Jack described it as “annoying, not painful,” like biting your cheek and waiting for it to heal.
Q2. How long before I can eat normally?
We advise a soft diet—think scrambled eggs and smoothies—for three days. By day 4 you can introduce pasta or fish. Crunchy tacos can wait two weeks. At Fortson Dentistry, we give a printed food timeline so you’re never guessing midday with an empty fridge.
Q3. Can grafts fail, and what then?
Failure is rare but possible if the graft loses blood supply or if sutures loosen. Smoking, grinding, and poor plaque control raise the risk. If a graft fails, we can often place a second graft once tissue stabilizes, usually at no extra fee under our warranty policy.
Q4. Is donor tissue safe?
Modern allografts are processed to FDA and AATB standards, removing cells yet preserving collagen. Studies show equal or better thickness gains compared to autografts. Patients who prefer to avoid a palate wound often choose this route without compromising results.
Q5. Will insurance cover a second opinion or outside referral?
Yes. PPO plans generally cover periodontal consultations. If you’re evaluating options, bring your x-rays. At our Soft Tissue Grafting page, you can request secure digital transfer so you’re not paying twice for imaging.

Here’s What We Tell Our Patients Before They Decide
Picture your gums as the cuff on a shirt sleeve. If that cuff unravels, the whole garment looks worn, and the threads below start fraying. Gum grafting re-sews that cuff before deeper damage sets in.
Most adults who commit to grafting wish they’d done it sooner—less sensitivity, more confidence, and the quiet relief of knowing their smile’s foundation is solid. Whether you’re like Jack, eyeing a half-marathon, or simply tired of wincing at ice water, soft tissue grafting can be a straightforward, life-improving fix.
Ready for clarity on your own gum health? Explore our detailed General Dentistry services, or reach out directly via our secure Contact Us form. We’ll review your gums, your goals, and your timeline—then map out a plan that feels right for you.
Ready to Transform Your Smile?
Book your visit today and enjoy personalized care, advanced technology, and a $70 New Patient Special — including full-mouth X-rays and a comprehensive exam. From Invisalign to dental implants, our expert team is here to help you smile with confidence.

BOOK AN APPOINTMENT
New patients only. The cost of a New Patient Appointment will be $150. Cannot be combined with any other offer or insurance. Limited time offer. Call (248) 557-8120 for details.

Thank you for booking your appointment!
We’ve received your request and will contact you soon to confirm the details. We look forward to seeing you at Fortson Dentistry South Lathrup.
